South Carolina to Utah on upping the ante on Medicaid cruelty: "Hold my beer."

I haven't written about Utah's batcrap Medicaid expansion program in quite awhile...since last March, in fact. As a reminder, here's where things stood at the time:
Yes, that's right: Not only did they lop 50,000 people out of the loop entirely, the other 90 - 100K enrollees will also be subject to...wait for it...work requirements. Well...sort of; keep reading.
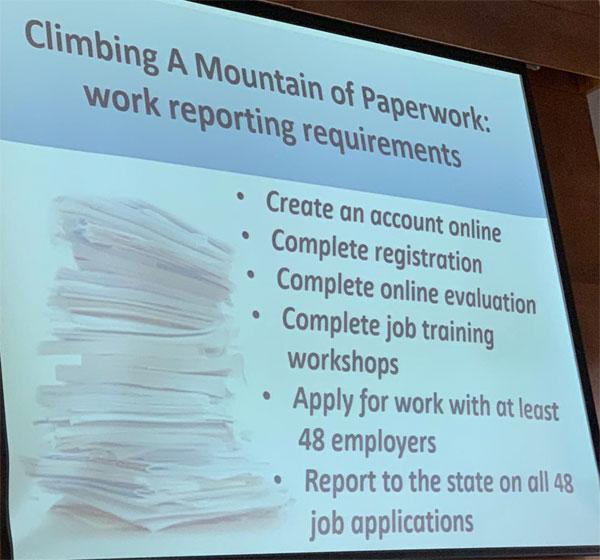
First, it looks like they'll have to apply to at least 48 employers as well. So...what, if they get hired by the first one they still have to apply with 47 more?
Note that it says "and" before the fourth item, not "or"...which means all of them will have to register online, complete a training assessment, apply to at least 48 companies and complete an online training course.
...Oh by the way, one more thing: The minimum wage in Utah is $7.25/hour.
- 30 hours/week x $7.25/hour = $217.50/week.
- $217.50 x 52 weeks = $11,310/year.
- For a couple, that's $22,620/year.
- 100% of the Federal Poverty Line for 2019 is $12,490/year for a single adult or $16,910/year for a couple.
I'm assuming FPL isn't calculated until after personal exemptions and the like are subtracted. If so, this is a moot point, but if not, it means a single adult who earns even 10% more than minimum wage wouldn't qualify for Medicaid expansion anyway...and a married couple who both worked 30 hours/week even at minimum wage would have no way of qualifying.
I'll be honest...I had completely forgotten about the "apply to at least 48 employers first" rule until yesterday, when Joan Alker, Executive Director of the Georgetown Center for Children and Families posted this reminder:
Here’s what Utah is going to require for its Medicaid expansion beneficiaries on 1/1/20 as a result of their unique work requirement.
Among other things, no coverage unless you’ve applied for a job w/ 48 employers. This will create huge coverage losses esp in rural areas.— Joan Alker (@JoanAlker1) December 11, 2019
This is pretty asinine, but at least these pointless, stupid work requirement jumping-through-hoops only apply to so-called "able-bodied" adults without children, right?
Well, South Carolina is apparently about to take the stupid and cruel to a whole new level. Also via Alker:
NEW: I’m deeply disturbed to share that tmrw at 11am the Gov of SC has scheduled a press conference in Greenville likely to announce that SC will be the 1st non Medicaid expansion state in the nation to receive approval for a work requirement. This will only affect poor parents.
— Joan Alker (@JoanAlker1) December 11, 2019
Read that again: South Carolina is a non-Medicaid expansion state. That means these work requirements will not impact "able-bodied adults without children"...but poor parents with children.
Here's who's eligible for Medicaid in South Carolina as of 2019:
- Children 0-1 (Newborns): 208% FPL
- Chidren 1-5 (Toddlers): 208% FPL
- Children 6-18: 208% FPL
- Pregnant Women: 194% FPL
- Parents/Caretakers: 62% FPL
- Adults w/no Children: n/a
Now, according to the waiver application itself, the following groups would be exempt from having to work 80 hours per month:
- Children enrolled in Medicaid or CHIP
- Members of federally recognized tribal organizations
- Pregnant women
- Disabled individuals
- Individuals over the age of 65
- Individuals who are the primary caregiver of a child or someone who is disabled
- Individuals receiving SSDI or SSI
- Individuals in alcohol/drug treatment programs
- Individuals receiving treatment for cancer
- Individuals meeting SNAP/TANF requirements
- Individuals who are determined by SCDHHS to be medically complex
OK, so children are officially waived, as are pregnant women and seniors, which are all good things. South Carolina never expanded Medicaid at all, so the last group doesn't apply. That leaves Parents/Caretakers of children under 18.
Except...South Carolina only allows Medicaid coverage for those folks up to 62% of the Federal Poverty Line to begin with. That's just $10,484/year if you're a single parent of one child...although supposedly it also exempts the "primary caregiver of a child", which I assume includes nearly all single parents by definition.
OK, so this really seems to only apply to the second parent...but again, for a family of 3 (2 parents, one child), the cut-off is just $13,224/year, or $1,100/month for the whole family.
As Alker notes, no matter how "reasonable" this may seem to be on paper (and it doesn't, at all, to me), in practice its pretty terrible:
To recap the situation: CMS Administrator Verma travels to SC today to announce the 1st Medicaid work requirement waiver in a non expansion state.
This shameless policy will exclusively target poor parents who are disproportionately women, black and living in rural areas— Joan Alker (@JoanAlker1) December 12, 2019
#2 There will be a small expansion for these parents which will be undercut by the work requirement on all poor parents that will cause thousands to lose coverage and won’t help them find work. Even short periods of uninsurance exposes the whole family to medical debt.
— Joan Alker (@JoanAlker1) December 12, 2019
#3 It will likely be said that kids are exempt - no need to worry! But kids are NOT exempt when their parents are harmed. Uninsured parents are more likely to have uninsured kids.
Meanwhile the nation’s uninsured rate for kids is on the rise.— Joan Alker (@JoanAlker1) December 12, 2019
UPDATE: Welp. It's official. Most of the state's waiver was approved...with some of it not approved:
Elements of the Demonstration Request that CMS is Not Approving at This Time
In its application, South Carolina requested to newly expand coverage to individuals ages 19 through 64 who meet the criteria for the P/CR group but who have incomes above the Medicaid standard of 62 percent of the FPL up to 95 percent of the FPL ( effectively 100 percent with the five percent income disregard) and who are not otherwise eligible for Medicaid.
In other words, SC tried to put a fig leaf on their work requirements by bumping that 62% cut-off up to 100%...but Trump's CMS said "nahhhhh."
Additionally, the state requested to newly expand coverage to a Targeted Adult Group of individuals ages 19 through 64, who otherwise would not be eligible for Medicaid, and who meet defined criteria that include being chronically homeless, justice involved, or needing substance use disorder (SUD) treatment. Unless such individuals are found to meet an exemption, the state requested that beneficiaries in the expanded P/CR group and the Targeted Adult Group also engage in qualifying community engagement activities for at least 80 hours per month, should they wish to opt into receiving Medicaid benefits. CMS is approving this request through a separate section 1115 demonstration approval, titled "Palmetto Pathways to Independence."
Hmmmm...ok, this is a bit confusingly worded, but it sounds like this expansion group was approved, just under a different waiver request...which means it was approved.
The state also requested to make changes to its TMA program. The state requested expenditure authority to provide financial assistance to those individuals that lost Medicaid coverage due to employment and who are also not eligible for employer-sponsored insurance to purchase a qualifying health plan on the Exchange. CMS is not taking action on these aspects of the state's proposal in this demonstration at this time.
Trump's CMS said "nahhhh" to this as well.
South Carolina also requested a number of eligibility and coverage changes for pregnant women and children. The state proposed to cover those eligible under the CHIP criteria for pregnant women with incomes from 194 percent FPL up to and including 241 percent FPL, covering the unborn population with up to and including 241 percent FPL, and covering those under age 19 that are eligible under CHIP criteria with incomes from 208 percent FPL up to and including 241 percent FPL. CMS is currently working with South Carolina to authorize coverage for these populations under Medicaid and CHIP state plan authority., but acknowledges that the state's request to cover these populations was included as part of the reforms CMS is approving today and may not have been pursued in isolation of the reforms being approved with this demonstration.
Ummm...huh? I can't figure out what this means...they want to approve these expansions, but can't because they were already approved anyway somewhere else in the approval? What?
The state requested to extend coverage beyond the postpartum period to women eligible for Medicaid based on pregnancy and to the mothers of children previously covered under CHIP. South Carolina ultimately revised its request, and CMS is approving 1,000 additional slots within the Targeted Adult Group under the Palmetto Pathways to Independence demonstration to prioritize coverage for pregnant women and parents of foster children, not otherwise eligible for Medicaid, needing SUD treatment and who meet specific eligibility criteria as described in the STCs.
So SC did ask to extend coverage for pregnant women after they give birth, and CMS said "no" but did bump out eligibility to 1,000 people for pregnant women, or something.
UPDATE 2: OK, hold on...apparently they did approve the "fig leaf" stuff in a separate waiver after all?? h/t Hannah Eichner:
Extent and Scope of the Demonstration
New Coverage for Parents
With this approval, South Carolina will newly provide coverage to individuals ages 19 through 64 who meet the criteria for the parent/caretaker relative (P/CR) group but who have incomes above the Medicaid standard of 62 percent of the federal poverty level (FPL) up to 95 percent of the FPL ( effectively 100 percent with the five percent income disregard) and who are not otherwise eligible for full Medicaid coverage, referred to as Population I in the STCs. As a condition of eligibility for choosing to opt into Medicaid and becoming newly enrolled, these individuals must, unless they are found to meet an exemption, engage in qualifying community engagement activities for at least 80 hours per month.
New Coverage for Targeted Adults
This approval also allows South Carolina to provide full Medicaid state plan benefits for 12 months to a Targeted Adult Group of individuals ages 19 through 64, who otherwise would not be eligible for Medicaid, and who meet defined criteria that include being chronically homeless, justice involved, or needing substance use disorder (SUD) treatment. Unless such individuals are found to meet an exemption, applicants to the Targeted Adult Group must also engage in qualifying community engagement activities for at least 80 hours per month, should they wish to opt into receiving Medicaid benefits. Beneficiaries in the Targeted Adult Group who are actively engaged in SUD treatment at the end of this 12 month period will have coverage extended for another 12 month period. Those beneficiaries who complete their 12 month period of eligibility and do not have coverage extended at the end of that 12 month period may reapply immediately and regain coverage under the Targeted Adult Group if the beneficiary meets the eligibility criteria, including the community engagement requirements, or is exempt from meeting the community engagement requirements, and if there is no waitlist for the Targeted Adult Group.
The state has also been given the flexibility to close enrollment in the Targeted Adult Group, if state appropriation is not adequate to cover the costs. When enrollment is closed, the state will continue to accept and review applications to determine whether applicants are eligible for Medicaid on any other basis. If the applicant is eligible for the Targeted Adult Group only, that applicant will be determined eligible but will be put into a suspended status until enrollment is re-opened. The state will maintain a waitlist to automatically enroll individuals the next time enrollment opens.
...Elements of the Demonstration Request that CMS is Not Approving at This Time
In its application, South Carolina requested to apply the community engagement requirements to the state plan coverage groups of P/CR and Transitional Medical Assistance (TMA). CMS is approving this request through a separate section 1115 demonstration approval, titled "Healthy Connections Works."
The state also requested to make changes to its TMA program. The state requested expenditure authority to provide fi nancial assistance to those individuals that lost Medicaid coverage due to employment and who are also not eligible for employer-sponsored insurance to purchase a qualifying health plan on the Exchange. CMS is not taking action on these aspects of the state's proposal in this demonstration at this time.
South Carolina also requested a number of eligibility and coverage changes for pregnant women and children. The state proposed to cover those eligible under the CHIP criteria for pregnant women with incomes from 194 percent FPL up to and including 241 percent FPL, covering the unborn population with up to and including 241 percent FPL, and covering those under age 19 who are eligible under CHIP criteria with incomes from 208 percent FPL up to and including 241 percent FPL. CMS is currently working with South Carolina to authorize coverage for these populations under Medicaid and CHIP state plan authority.
The state requested to extend coverage beyond the postpartum period to women eligible for Medicaid based on pregnancy and to the .mothers of children previously covered under CHIP. South Carolina ultimately revised its request, and CMS is approving 1,000 additional slots within the Targeted Adult Group to prioritize coverage for pregnant women and parents of foster children, not otherwise eligible for Medicaid, needing SUD treatment and who meet specific eligibility criteria as described in the STCs.
OK, it sounds like most of these were approved (or are "being worked on") after all, which is...better, I suppose, but all of th is is still pretty pointless.
If you take the specific exemptions at face value, it sounds like they're going through an awful lot of fuss and bother simply to target a handful of supposed "couch potato" spouses or whatever.