California: Final 2020 ACA Open Enrollment Tally: 1.54 million QHPs, up 1.6% y/y
When I last checked in on Covered California a couple of weeks ago, they still had two days left before their 2020 Open Enrollment deadline, and had managed to rack up 1.51 million on-exchange enrollments. This included 1.15 million renewals of existing enrollees, plus another 364,000 new enrollees.
I noted at the time that they had just barely beaten 2019's total with two days to go, and would have to add about 7,500 more to break 2018's total, and another 43,000 to beat 2017.
Well, they ended up in between the two, partly due to an overestimate of the renewal figure:
New California Policies Make Huge Difference, Increasing New Signups During Covered California’s Open Enrollment by 41 Percent
New Special-Enrollment Period Announced to Continue to Get Word Out on New Subsidies and Penalty
- A total of 418,052 people newly signed up for coverage during Covered California’s open-enrollment period, which is 41 percent higher than last year’s figure of 295,980.
That's 54,000 additional new enrollees added in the final two days of Open Enrollment.
- New state policies, which provided additional money to help people purchase health insurance and established a state penalty, were key components that led to Covered California’s highest new enrollment total since 2016.
- The strong total shows how California is building on the Affordable Care Act, enrolling healthy consumers and saving money for Californians, in contrast to federal policies that have led to higher premiums and millions losing coverage.
- Covered California is announcing a special-enrollment period through April 30 to address concerns that many Californians remain unaware of the new financial help or the new state penalty.
Hmmmm....the Special Enrollment Period is interesting. HealthCare.Gov and some state exchanges did something like this in spring 2015 (the first year people had to actually pay the mandate penalty) and managed to get around 210,000 more enrollees. Of course, the penalty for 2014 was only $95 or 1% of income at the time. This year, the District of Columbia is apparently doing something similar with their local mandate penalty as well.
SACRAMENTO, Calif. — Covered California announced that 418,052 people had newly selected a health plan for 2020 during the most recent open-enrollment period, which formally closed on Jan. 31. The total is more than 122,000, or 41 percent, higher than last year’s figure of 295,980. The increase comes after the state of California instituted two key policies designed to help and encourage more people to become insured: reinstituting a penalty for those going without coverage, which had been lowered to zero by federal action in 2019 and adding state subsidies to build on and go beyond the Affordable Care Act’s financial help.
“Californians are seeing that by building on — instead of undercutting — the Affordable Care Act, they are directly benefiting from lower health care costs and more people being insured,” said Covered California Executive Director Peter V. Lee. “The new enrollment that occurs during each year’s open-enrollment period is vital to getting more people covered and keeping costs down by enrolling a healthy risk mix. This dramatic rebound in new enrollment shows how effective state policies can make quality coverage more affordable and encourage people to get covered.”
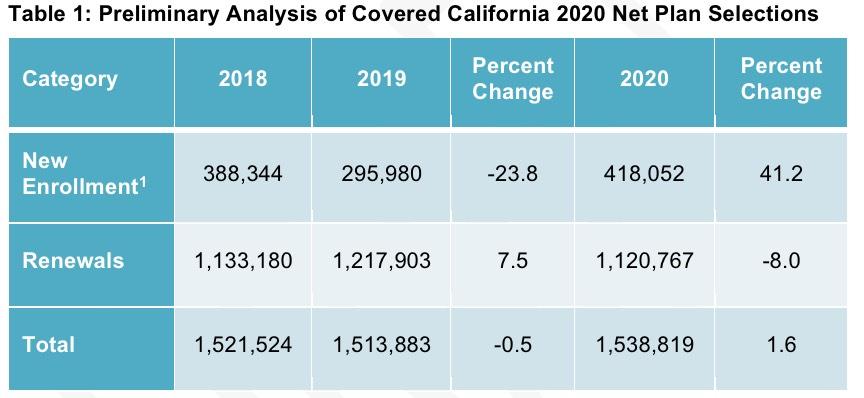
Preliminary analysis shows that the total number of net plan selections for 2020 is 1,538,819, which reflects 1,120,767 consumers renewing their coverage and 418,052 consumers newly signing up for coverage during open enrollment. Overall, there are 24,936 more plan selections compared to 2019, an increase of almost 2 percent (see Table 1: Preliminary Analysis of Covered California 2020 Net Plan Selections).
As I noted above, they tacked on 54,000 additional new enrollees in the final two days. However, the number of renewing enrollees was 29,000 fewer than they had previously estimated, so they ended up 25,000 higher than I previously thought.
New State Policies and Effective Outreach Drive New Enrollment
California adopted several policies to pursue Gov. Newsom’s stated goal of moving toward universal coverage, including two that were specific to the individual market:
- Effective January 2020, California required its residents to have health insurance coverage — reinstating the federal penalty that was integral to the Affordable Care Act. Those who can afford coverage but choose to go without it could face a penalty when they file their taxes with the California Franchise Tax Board in 2021. The penalty can be more than $2,000 for a family of four.
- California launched a state subsidy program that expanded the amount of financial help available to many consumers, including a first-in-the-nation program to help middle-income consumers afford coverage. The new state subsidies could extend to an individual making up to $74,940 and a family of four with a household income of up to $154,500.
- California extended its open-enrollment period through Jan. 31, compared to Jan. 15 last year — in dramatic contrast to the federal decision to have open enrollment close on Dec. 15.
Covered California and the Franchise Tax Board (FTB), which will be implementing the penalty, worked to get the word out about these new policies throughout open enrollment. Elements of the robust marketing and outreach included Covered California:
- Investing $121 million in statewide marketing and outreach during the current fiscal year.
- Supporting more than 10,000 Certified Insurance Agents across the state and more than 100 community organizations that were recipients of Covered California’s Navigator grants totaling $6.5 million.
- Conducting more than a dozen phone banks on in-language television stations across the state targeting English, Spanish, Mandarin and Hmong speakers.
- Partnering with social media influencers such as Laila Ali, Leo Santa Cruz, J.R. Todd, Nathan Adrian and others to create content that has generated more than 3 million impressions.
In addition, Franchise Tax Board has worked with Covered California to get the word out, including:
- Working with tax-filing software companies to include penalty information that consumers will see when they file their taxes.
- Conducting outreach and training for tax professionals.
- Sending mail to more than 2 million households alerting them to the penalty and telling them how to get coverage.
New State Subsidies Helping Over 625,000 Californians Lower Their Health Care Costs
Through the open-enrollment and renewal periods, about 625,000 new and renewing consumers qualified to receive the new state subsidies.
State Subsidies That Complement Federal Assistance for Those Earning From 200 to 400 Percent FPL
About 576,000 lower-income consumers, who earn between 200 and 400 percent of the federal poverty level (FPL), will receive an average of $608 per month per household in federal tax credits and new state subsidies (which averages $23 per household). The financial assistance lowers the average household monthly premium from $881 per month to $272, a decrease of 70 percent.
OK, that's 576,000 people receiving $23/month per household, or $276/year. It's important to note that's per household, not per person. Assuming 1.4 people per policy (CoveredCA's historic average, which is smaller than the average household size nationall for several reasons), that's around $197/enrollee, or $113.4 million in subsidies. Of course, that assumes 100% effectuation every month; historically it usually averages around 80% of the official OEP total, so let's call it $91 million in state subsidies for this crowd this year, give or take.
First-in-the-Nation State Subsidies for Middle-Income Consumers
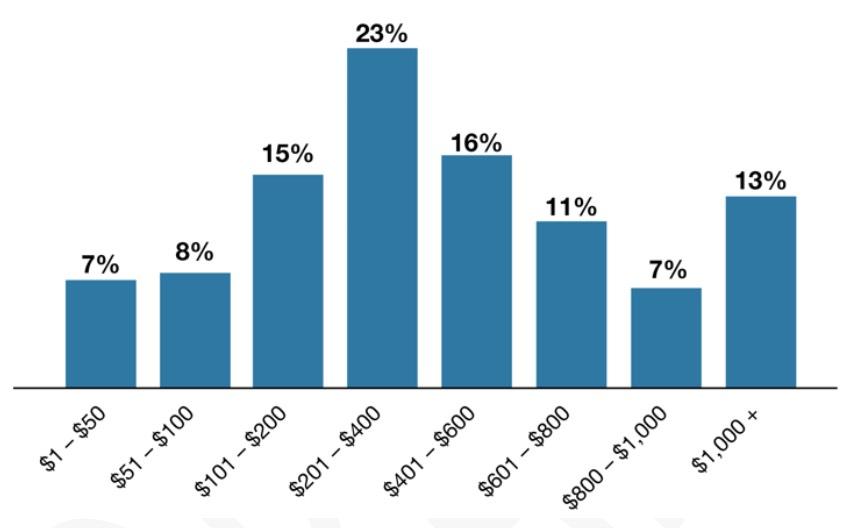
Nearly 32,000 middle-income consumers who were previously ineligible for any federal support because their household income was above the federal “cliff” of 400 percent of the FPL qualified for new state subsidies. The new financial help went to about 47 percent of consumers applying in the 400 to 600 percent FPL income bracket. The average state subsidy to eligible households is $504 per month, lowering their monthly premium by nearly half (see Figure 1. Distribution of California State Subsidies Among Eligible Middle-Income Households [400 to 600 Percent FPL]).
Again, that's per household, not per enrollee. Let's call it $360 per enrollee per month, or $4,320 in subsidies per enrollee per year, times 32,000 enrollees. That's around $138.2 million for the year. Take 80% of that and it's more like $110 million give or take.
Combined with the 200-400% recipients, and California should be paying out roughly $201 million in state subsidies this year.
Figure 1: Distribution of California State Subsidies Among Eligible Middle-Income Households (400 to 600 Percent FPL)[2]
“The average state subsidy for eligible middle-income Californians — who up until now were not eligible for any assistance — was $504 per month. But it’s even more striking that more than one in 10 of those receiving help had their monthly premium lowered by over $1,000,” said Lee. “The new state subsidies are making a huge difference to families across California.”
Covered California also reported that an estimated 280,000 Californians, likely eligible for new state or existing federal subsidies, kept their “off-exchange” coverage and did not get the financial help that would make it easier to afford and keep their coverage. Most of these individuals earn under 400 percent of the federal poverty level and would be eligible for both the state and federal subsidy, while about 40,000 would be eligible to receive the new state subsidies for middle-income Californians.
Holy crap. Let me repeat that: There's 280,000 Californians who are currently paying full price for ACA-compliant individual market policies who would be eligible for an average of $7,300/year per household (around $5,200 apiece) if they simply enrolled in an on-exchange policy instead...and another 40,000 who are likely eligible for an average of over $6,000/household ($4,300 per enrollee) if they did so.
If my math here is correct, that means there's around 320,000 Californians who are leaving an average of around $5,100/year in rebates apiece on the table.
If you assume that, say, 90% of these folks are eligible (not everyone earning <400% FPL is...it still varies greatly depending on your age, income, household size and where you live), that's still upwards of 290,000 who are leaving up to $1.5 BILLION on the table.
“The penalty helped drive down premiums for everyone in the individual market, and new state subsidies are already helping more than 600,000 people save even more on their health insurance,” Lee said. “However, we are still hearing that far too many people do not know about these policies, so Covered California wants to continue to get the word out and give them more time to learn about the penalty and how affordable coverage can be.”
Drop in Renewals Driven by Low New Enrollment for 2019 Following the Penalty Removal
The significant increase in new enrollment was partially offset by an 8 percent decrease in the number of renewing consumers. Covered California’s preliminary analysis points to several potential reasons for the reduction in renewals relative to 2019. As noted above, 2019 marked the first year that the federal government zeroed out the individual mandate penalty, which led to a sharp decrease in the number of new consumers signing up for coverage during last year’s open-enrollment period. Historically, a decrease in new enrollment translates to a decrease among renewing consumers because there are fewer consumers in the system to carry forward into renewal. Covered California entered this renewal season with nearly 40,000 fewer members covered in October 2019 (for 2020 coverage) than it did in October 2018 (for 2019 coverage).
“Covered California’s preliminary analysis of the reduction in the number of consumers renewing appears to be another result of the federal decision to remove the penalty that resulted in fewer people eligible to carry their coverage into 2020,” Lee said. “What we have seen this open-enrollment period only affirms the bold decision of the governor and the state Legislature to provide that economic nudge that some people need to get health insurance.”
New Special-Enrollment Period Announced
Covered California also announced that effective Feb. 18 it will establish a special-enrollment period for those who were unaware of the state penalty or the new financial help. Consumers who fall into those categories, or who are currently insured off exchange (directly through an insurer) and want to switch to Covered California to benefit from the new state subsidies, will have through April 30 to sign up for coverage.
Covered California made the decision after gathering information throughout open enrollment and after the close of enrollment. In December, Covered California surveyed the public and found a significant percentage of the uninsured were unaware of the new financial help or penalty. Based on those findings, Covered California began looking at whether a special-enrollment period would be warranted. In the first week of February, Covered California surveyed 10,000 of its Certified Insurance Agents and found that there is still a substantial lack of awareness, with 41 percent saying only some or none of their consumers knew about the penalty, and 80 percent saying the penalty is motivating or extremely motivating for their consumers.
“I encourage everyone who does not have qualifying health insurance to take advantage of the special enrollment period and secure coverage now. I like signing tax refund checks, not assessing penalties,” said State Controller and FTB Chair Betty T. Yee.
...Covered California will be launching a new campaign to publicize the special-enrollment period, starting this month with social media messaging and consumer emails. Television ads in English and Spanish will start on March 9. Also starting that day will be radio and digital ads in English, Spanish, Mandarin, Cantonese, Korean and Vietnamese. This marks Covered California’s first use of television ads to promote a special-enrollment period.
“We know that there are hundreds of thousands of people, both low income and middle income, who are insured off exchange but could be saving significant amounts of money if they switch to Covered California to benefit from federal financial help or new state subsidies, or both,” Lee said. “Covered California is working with everyone it can to put consumers first by maximizing the amount of time that people can get covered and minimizing the number of people who are subject to a penalty.”
During this special-enrollment period, consumers will be able to sign up at any point and will be covered on the first of the following month.
Comparing Covered California to States Served by the Federally Facilitated Exchange
California’s instituting the new policies for 2020 had impacts well before open enrollment began. In particular, the new state policies helped Covered California negotiate a rate change of only 0.8 percent for 2020, which is the lowest in the exchange’s history. This historically low premium increase was largely driven by health insurance companies’ pricing based on the assumption and hope that the reinstatement of the penalty would lead to larger (and healthier) enrollment. This led to lower costs for those who do not get subsidies and for the federal government due to its being able to make lower Advanced Premium Tax Credit payments.
“We know the penalty is not popular, but it is the law and it is leading to more people covered, a healthier consumer pool and lower premiums for everyone,” Lee said.
In addition, California’s consumers continue to benefit from robust competition among carriers. In 2020, not only will nearly all consumers be able to choose from two or more plans, but 75 percent will have four or more choices, and more than half of consumers (56 percent) will be able to choose from five plans or more.
In addition, Covered California invested $121 million in marketing and outreach to help it maintain a consumer pool is a continuation of a policy that has contributed to California consistently having a “risk score” approximately 20 percent below the national average for the individual market, which has likely to have saved enrollees and the U.S. Treasury an estimated $12.5 billion over the past five years.
The actions and policies of California and of Covered California are in stark contrast to those seen at the federal level, which has maintained its significant cutbacks in marketing and outreach while encouraging consumers to enroll in substandard coverage in the 38 states served by the federally facilitated exchange (FFE). These policies have been demonstrated to directly contribute to far higher premium increases and lower new enrollment in states relying on the federal marketplace and dramatic drops in enrollment of unsubsidized consumers “off exchange” in those states.
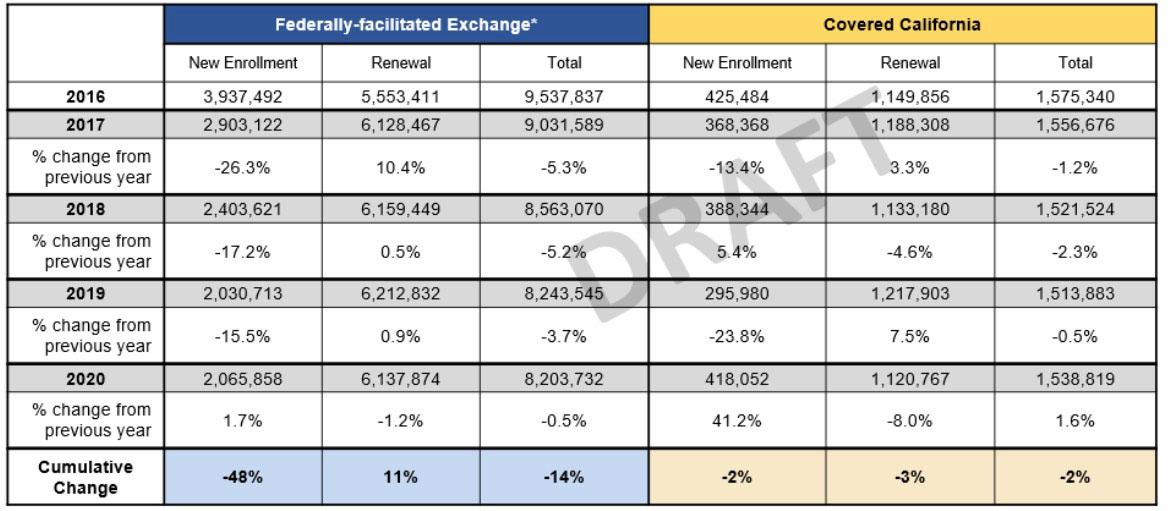
New enrollment in those states that rely on the FFE has dropped 48 percent since 2016, which represents a reduction of nearly 1.9 million people. Covered California’s new enrollment remained relatively stable (see Figure 2: Comparing New Enrollment in Covered California and FFE, 2016-2020).
Figure 2: Comparing New Enrollment in Covered California and FFE, 2016-2020[3]
Overall, the enrollment of consumers in states served by the federally facilitated exchange has declined by over 1.2 million compared to 2016. During the same time period, Covered California’s total enrollment has remained relatively stable. (see Table 2: Comparing Net Plan Selections in Federally-Facilitated Exchange States and California, 2016-2020).
Table 2: Comparing Net Plan Selections in Federally-Facilitated Exchange States and California, 2016-2020
“Fostering stable marketplaces that work for consumers is not a one-year proposition,” said Lee. “What we see over the past three years is the direct impact of concerted efforts to undercut and impede the policies of the Affordable Care Act. California’s experience shows that the policy of protecting and building on the Affordable Care Act is leading to lower costs and more people covered.”
The loss in FFE enrollment comes in addition to a steep reduction in the number of unsubsidized consumers in the individual market nationally. As Covered California noted in its report “Covered California’s First Five Years: Improving Access, Affordability and Accountability,” unsubsidized enrollment in the individual market fell 44 percent between 2016 and 2018.
[1] The open enrollment number includes consumers who had coverage off exchange and switched to on-exchange coverage to benefit from new subsidies. Even after subtracting the entire newly enrolled 400 to 600 percent federal poverty level (FPL) population, Covered California’s new signups in 2020 would still be 36 percent higher than in 2019 and still the highest total since 2016.
[2] Average is among those receiving state subsidies. Consumers in 400 to 600 percent FPL with a benchmark that costs less than “required contribution” of income are not included.
[3] Analysis of FFE states includes the 32 states served by the FFE and the six states with state-based exchanges facilitated by the federal platform (SBE-FP). We exclude Kentucky and Nevada from all counts due to these states switching marketplace types in 2017 and 2020, respectively. All FFM data are from CMS public data releases. FFM totals exclude Kentucky and Nevada for changes in marketplace type that occurred over the period shown.