Oh Yeah...I almost forgot The Graph!
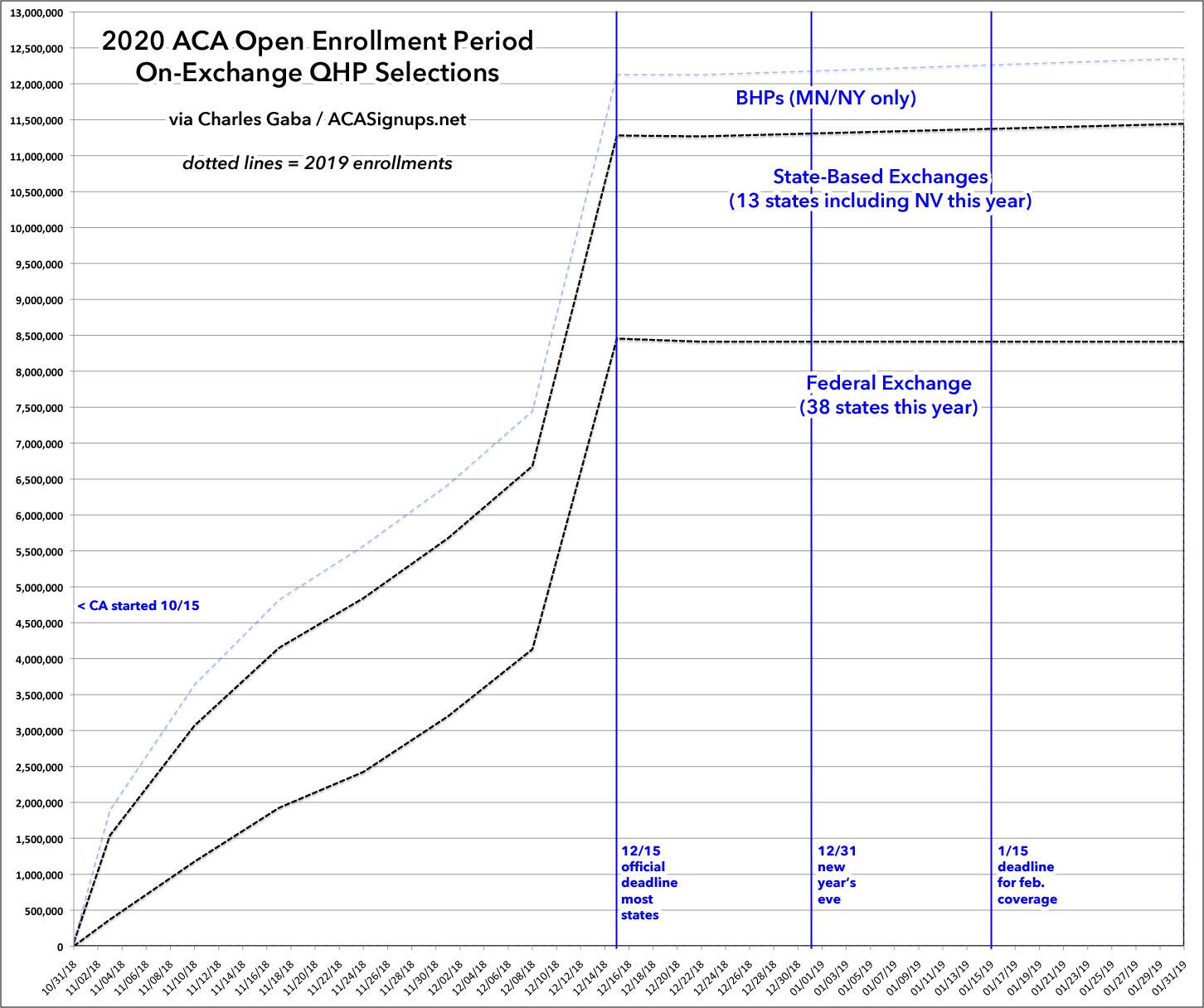
The original purpose of this website was, of course, to do real-time (or close to real-time) tracking of how many people actually select Qualified Health Plans (QHPs) via the ACA exchanges.
Every year I start out with a "blank" with my projections for how I think the upcoming Open Enrollment Period (OEP) will play out. For 2020, however, I'm just overlaying 2019's enrollment patterns on the graph (for both the federal and state exchanges) to see how things play out year over year.
There's some important things to keep in mind for the 2020 OEP:
- California's expanded/enhanced premium subsidies should juice up enrollment, especially for people in the 400-450% FPL income range.
- California also reinstated the individual mandate penalty, which should also help a bit.
- Rhode Island also reinstated the mandate penalty this year, joining Massachusetts, New Jersey and DC, all of which already reinstated it locally last year.
- Nevada split off from the federal exchange (HealthCare.Gov) onto their own state-based exchange. As a result, I'd expect the HC.gov numbers to be slightly lower...and the State-based exchange totals to be slightly higher (duh!).
- Several more states (Colorado, Delaware, Montana, North Dakota, Rhode Island & Wisconsin) instituted ACA Section 1332 reinsurance waivers this year, which should boost unsubsidized enrollment...but will also likely hurt subsidized enrollment to some degree as the Reverse Silver Loading effect will likely be felt strongest in those states.
- Idaho, Utah and Nebraska all kind-of, sort-of implemented Medicaid expansion programs (although the state legislatures/governors tried to water them down as much as possible). This will have a negative effect on exchange enrollment since enrollees earning 100-138% FPL will be shifted off of heavily-subsidized ACA exchange plans over to Medicaid instead.
THE BIGGEST WILDCARD is, of course, the 5th Circuit Court of Appeals ruling on the Idiotic Texas Fold'em (Texas vs. US) lawsuit, which is expected to be announced literally at any moment. While the ruling will be immediately appealed up to the U.S. Supreme Court regardless of what the decision is (unless they kick it back to the original judge to review again), the news of their ruling will still cause tremendous confusion and panic, especially if they rule that the law should be struck down entirely or in large part.
If that happens, it will cause some people not to enroll at all (assuming their coverage will be dropped mid-year, which isn't what would happen), while it could cause others to enroll who wouldn't have otherwise (assuming this is their Last Chance to qualify for affordable healthcare coverage before it all goes away). Who knows?
What will the overall impact be on enrollment of all these factors? Well, the trend since the all-time high enrollment period in 2016 (12.7 million total QHP selections) has been for federal exchange enrollment to drop by several hundred thousand each year...while state-based exchange enrollment increased by a percent or two. Obviously I'll have to correct for Nevada shifting from the former to the latter status.
Will this trend continue this year? I'm not making any predictions this time around.